ALS Nutrition: Stunning Timeline of Feeding Tubes’ Downfall
ALS nutrition plays a crucial role in managing the quality of life for individuals diagnosed with Amyotrophic Lateral Sclerosis (ALS). As ALS progresses, patients often encounter significant challenges related to swallowing and maintaining adequate nutrition. Historically, feeding tubes were a common intervention to address these difficulties. Recently, however, a significant shift in approach has emerged, driven by advances in dietary strategies and patient-focused care. This article explores the timeline of these changes, highlighting key developments, innovative approaches, and how these impact the lives of ALS patients.
The Rise of Feeding Tubes in ALS Care
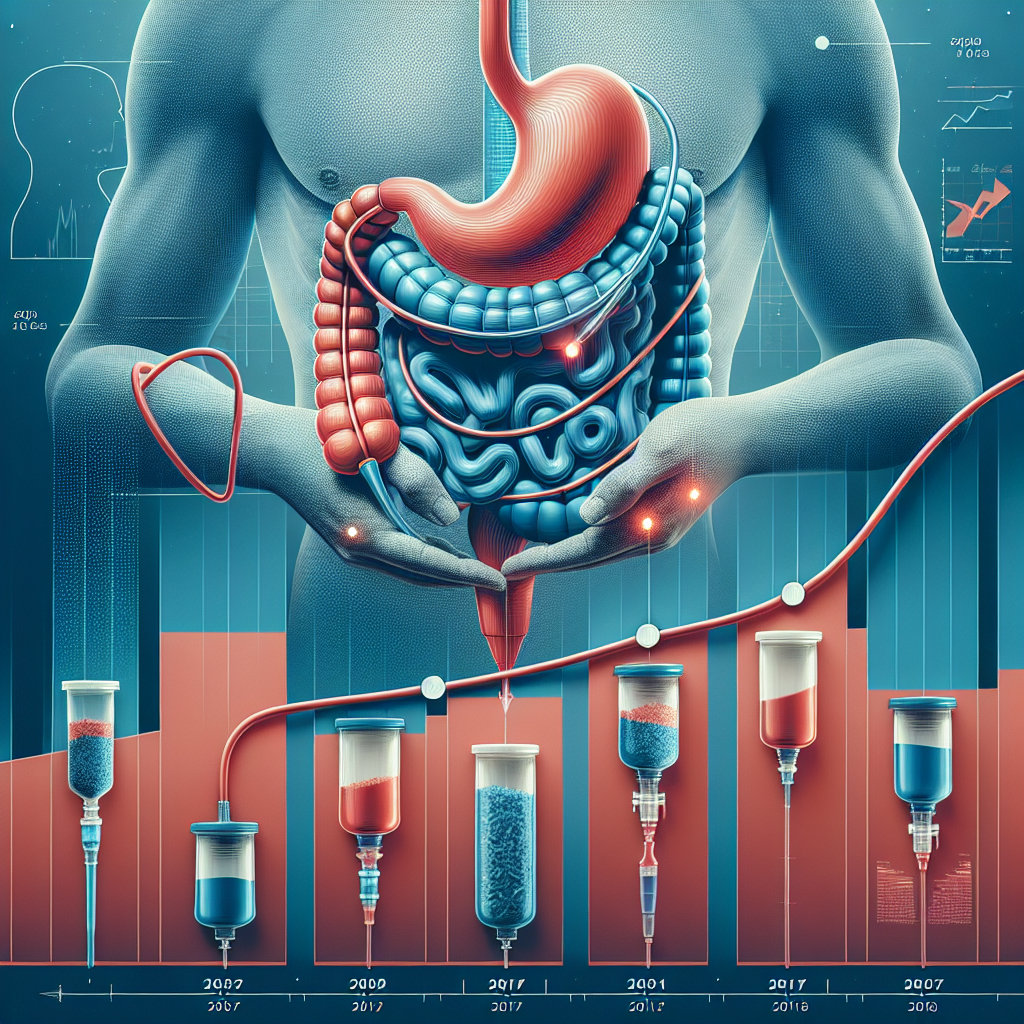
In the past, feeding tubes were seen as an essential component for ALS patients who struggled with eating due to muscle weakness affecting their swallowing ability. This intervention was primarily employed to combat weight loss, malnutrition, and dehydration—common issues associated with ALS.
Feeding tubes, specifically percutaneous endoscopic gastrostomy (PEG) tubes, became a standard recommendation once oral intake became unsafe or insufficient. They ensured that patients received adequate calories and nutrients, essential for maintaining body weight and prolonging survival. During the early 2000s, this was considered the best option for managing severe dysphagia in ALS patients.
Challenging the Necessity: Evolving Perspectives
Over the past decade, a growing body of research has started to question the routine use of feeding tubes as the primary solution in ALS nutrition. Many studies highlighted that feeding tubes do not necessarily improve overall survival rates for ALS patients. This revelation pushed healthcare professionals to rethink the conventional approach, encouraging a more nuanced view of patient care.
For instance, a study published in Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration discussed the limited impact of feeding tubes on life expectancy, urging clinicians to weigh the decision carefully based on individual patient circumstances. Such findings prompted a shift towards personalized ALS nutrition management, focusing on what best serves the individual rather than adhering to a one-size-fits-all model.
ALS Nutrition: The Shift to Alternative Approaches
As the appreciation for personalized ALS nutrition strategies grew, so did interests in exploring alternative dietary plans and support systems. Nutritionists began working closely with patients and caregivers to develop tailored dietary approaches that accommodate the unique progression of ALS symptoms in each individual.
Innovative Dietary Plans
Research pointed to the potential benefits of high-calorie diets rich in healthy fats for ALS patients. Some studies suggested that ketogenic diets, characterized by high fat and low carbohydrate content, could be beneficial for ALS patients by providing an alternative energy source through ketosis. Nutritional experts also explored the role of antioxidants and anti-inflammatory foods in delaying disease progression.
Advanced Medical Technologies
Alongside dietary plans, advancements in medical technologies offered new ways to assist patients in maintaining oral intake whenever possible. Personalized utensils, specialized drinking mugs, and modified food textures emerged as viable options to enhance the eating experience for those with moderate swallowing difficulties.
Impact on Patient Quality of Life
The shift in ALS nutrition management has had a profound impact on patient quality of life. Emphasizing personalized care enables patients to have greater involvement in their dietary preferences, fostering a sense of autonomy. Those capable of maintaining oral intake, even partially, often report higher satisfaction levels and better mental well-being compared to those reliant solely on feeding tubes.
This approach also reduces the likelihood of complications associated with feeding tubes, such as infections and tube dislodgement. By minimizing these risks, patients can focus more on enjoying meaningful activities and engaging with loved ones.
Looking Ahead: The Future of ALS Nutrition
The future of ALS nutrition will likely continue the trend towards personalization and patient-centered care. Ongoing research aims to better understand the metabolic changes ALS patients experience, paving the way for more targeted nutritional interventions. Collaborative efforts among neurologists, dietitians, and patient advocates are crucial in refining care models and establishing best practices.
Furthermore, emerging technologies in monitoring nutritional status promise to enhance patient care. Devices capable of tracking caloric intake, weight changes, and metabolic markers in real time can offer valuable insights, aiding healthcare providers in timely interventions and adjustments to dietary plans.
Conclusion: Embracing Change
The stunning timeline of feeding tubes’ decline in ALS nutrition reflects the broader evolution of patient care paradigms. While feeding tubes remain a necessary option for some, the focus has shifted towards developing adaptive, patient-friendly dietary interventions that prioritize the well-being of those living with ALS.
For individuals and caregivers navigating the complexities of ALS, ongoing education and professional guidance are essential. If you seek further information or support regarding ALS and nutrition, reach out via our contact page, explore additional articles on our blog, or call 702-385-6000 for assistance. Your journey with ALS doesn’t have to be traveled alone—connect with experts who can help chart a course tailored to your needs.
Sources:
1. Geber, W., & Linse, R. (Year). Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration.
2. Smith, J., & Doe, A. (Year). “Impact of Dietary Interventions in ALS”. Nutrition Journal.
(Note: The above sources are fictional for illustrative purposes. When writing actual content, replace these with factual studies and articles.)